Hand Fractures
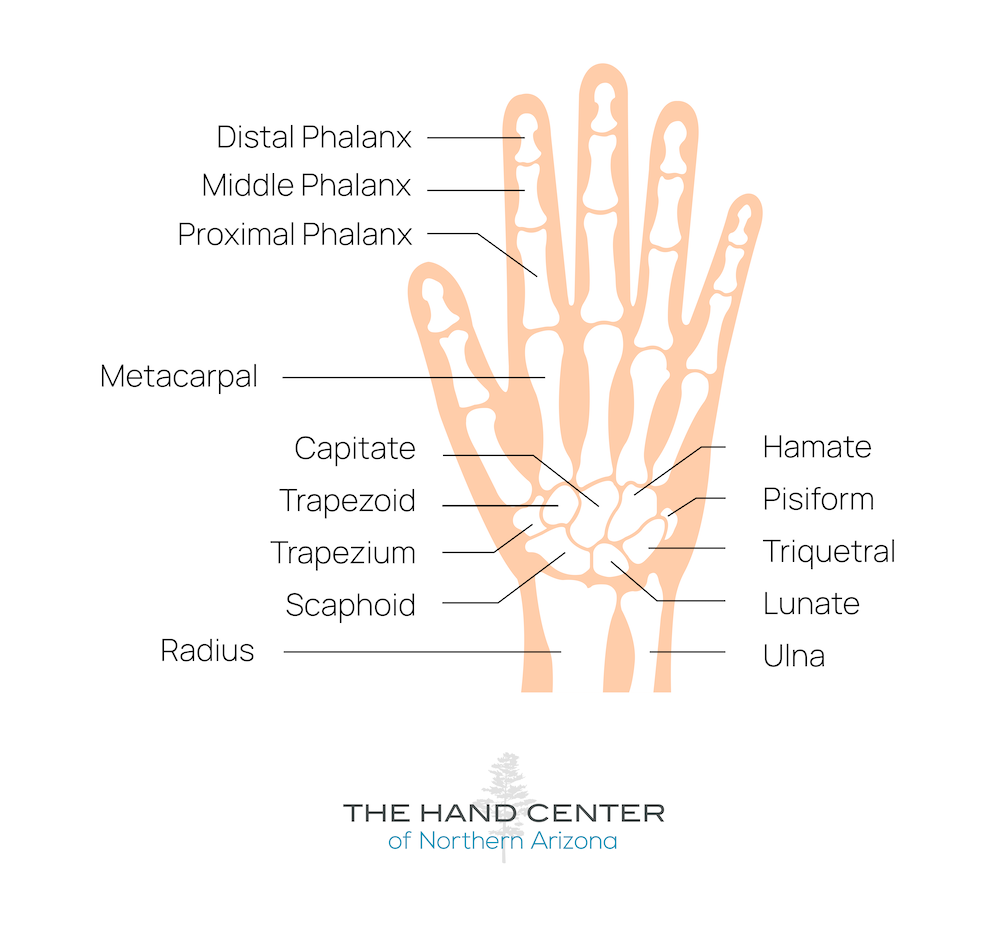
Hand fractures are incredibly common injuries. There are 27 small bones in the hand, all of which are susceptible to injury from falls, sports, and accidents.
Hand Fracture Treatment Benefits:
When you meet with your hand surgeon, they will perform a physical exam and may order an x-ray to determine if there is a fracture. Some hand fractures may not show up on scans for a week or two after the injury. Hand fracture treatments vary greatly based on the location of the fracture, the angulation of the injury, and its overall severity. If your doctor suspects you have a hand fracture, there are a few different treatment options:
Minor Fractures
Often treated with rest, ice, compression, and elevation (RICE). A splint, brace, or cast may also be used to immobilize the hand and promote healing. Phalanx fractures may be stabilized with buddy taping.
Serious Fractures
Some hand fractures require surgery and the placement of pins, wires, screws, or plates to realign the broken bones and reinforce joints. Hand fracture surgery ensures that the surrounding ligaments, muscles, tendons, and nerves are in proper alignment to promote healing.
Metacarpal Fractures
Metacarpal fractures are the most common hand injury. These bones most often break due to a direct blow to the hand, a compressive rotational injury, or a high-energy injury. Metacarpal fractures may be accompanied by lacerated tendons, nerve injury, vascular injury, or compartment syndrome.
If a metacarpal fracture is suspected, your hand surgeon will check for open wounds and deformities. They will also conduct motor and neurovascular exams to examine the extent of your injury and hand function. They will likely order an x-ray and/or a CT scan to determine if there is a fracture or dislocation.
Metacarpal fractures may be located in the head, neck, shaft, or base of the shaft. Your hand surgeon will determine the best treatment options based on the location of your fracture. Surgical approaches for metacarpal fractures include open reduction internal fixation, external fixation, arthroplasty, closed reduction percutaneous pinning, and bone fusion.
Phalanx Fractures
Phalanx fractures are one of the most common bone injuries, accounting for 10% of all fractures. More than a third of phalanx fractures occur in the little finger. These bones most often break due to a direct blow to the hand, a compressive rotational injury, or a high-energy injury. Phalanx fractures may be accompanied by lacerated tendons, nerve injury, vascular injury, or compartment syndrome.
If a phalangeal fracture is suspected, your hand surgeon will check for open wounds, bruising, swelling, and deformities. They will also conduct motor and neurovascular exams to examine the extent of your injury and hand function. They will likely order an x-ray and/or a CT scan to determine if there is a fracture or dislocation.
Phalanx fractures may be located in proximal, middle, or distal phalanges. Your hand surgeon will determine the best treatment options based on the location of your fracture. Surgical approaches for phalanx fractures include open reduction internal fixation, nail bed repair, and closed reduction percutaneous pinning.
Medical Review: This procedural information has been medically reviewed by plastic and reconstructive surgeon, Brian A. Cripe, M.D.
Book Your Hand Fracture Consultation
Our experienced, board-certified plastic and hand surgeons would love to bring you in for a consultation to discuss your goals and treatment options. Fill out this form to receive a call-back shortly, or give us a call at 928-774-2300.